

MC3 Pediatric Medical Director

MC3 Perinatal Medical Director
As a child psychiatrist, we sometimes hear our trainees and colleagues say, “We can understand working with children, but how do you manage the parents?!”
This question underscores why MC3 supports both providers caring for children and those who care for new mothers and infants. The tenets of Infant Mental Health inform much of what we do in MC3. It is in the earliest years of life that relationships are built, and the “dance” between parents and their children can be most easily taught.
We know that if parents can learn how to read their children’s cues — “What is my child feeling behind this difficult behavior?” and “What does he need from me?” — they’ll be well on their way to supporting their child in developing a secure attachment relationship. This attachment security is an important ingredient in the “secret sauce” that helps children develop emotional regulation and resilience regardless of what challenges they might have.
On the other hand, parents who have mental health or addiction issues or who themselves experienced traumatic childhoods are at risk for perpetuating this pattern. If they didn’t get what they needed while growing up, how can they possibly know how to give it to their child?
To give children what they need, parents need to feel supported, nurtured, and “held” by the health care providers caring for their children. They need to feel heard and understood and not blamed for their children’s illnesses. Providers may sometimes need to “catch the parent doing something right” and call it to their attention, as well as to point out the smile, the touch, the leaning in that children naturally do with their parents to let them know “you are my person.”
This is why our consultations are infused with the tenets of Infant Mental Health and Early Childhood and Relational Health. These relationally, developmentally, and culturally-informed principles are built into the consultations, educational offerings, and resources we offer to providers in primary care settings, schools, and soon, emergency settings.
We feel that when we can instill these principles early, it gives providers the tools they need to care for the parents so that they can care for their children. Whether the children are preschoolers, adolescents, or young adults, the principles are the same.
We are proud to highlight some of the “best of” from the past year and we look forward to working with you in this year ahead. Here’s to good physical and emotional health for our providers and those they care for. We wish all of you the best in 2025.
Reflecting on the progress and impact captured in this report, I’m inspired by the strides we’ve made together and reminded of the work still ahead. Your partnership is vital as we navigate the challenges of supporting maternal mental health in Michigan.
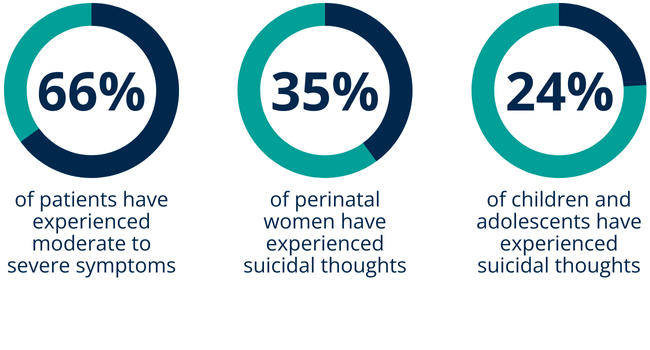
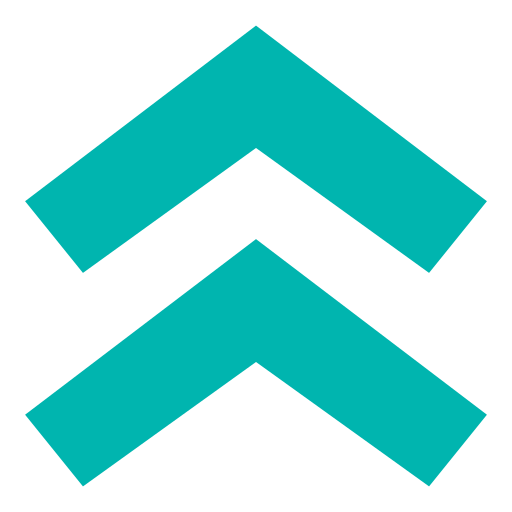
The maternal health crisis in the United States is a sobering reality. Mental health conditions — including depression, suicide, and overdose — are the leading preventable causes of death in the postpartum year. Yet, despite these alarming trends, Michigan faces a severe shortage of perinatal psychiatrists and therapists to provide specialized care.
Earlier this year, the Policy Center for Maternal Mental Health designated multiple rural and urban counties in Michigan as Maternal Mental Health Dark Zones, areas where high-risk populations coincide with significant resource gaps. Michigan has the unfortunate distinction of being among the top six states with the most critical maternal mental health disparities.
This crisis is compounded by broader maternity care shortages. Eighteen percent of Michigan counties have been described as maternity health care deserts. In rural Michigan, the situation is even more dire — 45% of rural counties in Michigan have limited or no access to maternal health care. The consequences are stark: the burden on the remaining providers from all professional backgrounds grows heavier, and the gaps in care widen.
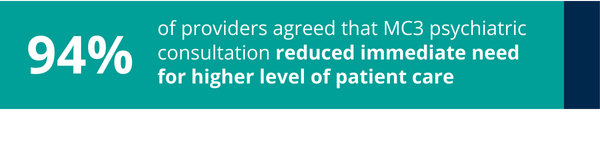
This reality demands innovative, collaborative solutions. Programs like MC3 exemplify how we can rise to meet these challenges. By providing same-day psychiatric consultations and resources for providers, MC3 ensures timely, evidence-based mental health care for pregnant and postpartum individuals. The data support that this model works: It not only alleviates the strain on providers but also improves outcomes for families, demonstrating that investing in care coordination, provider education, and community connection pays off.
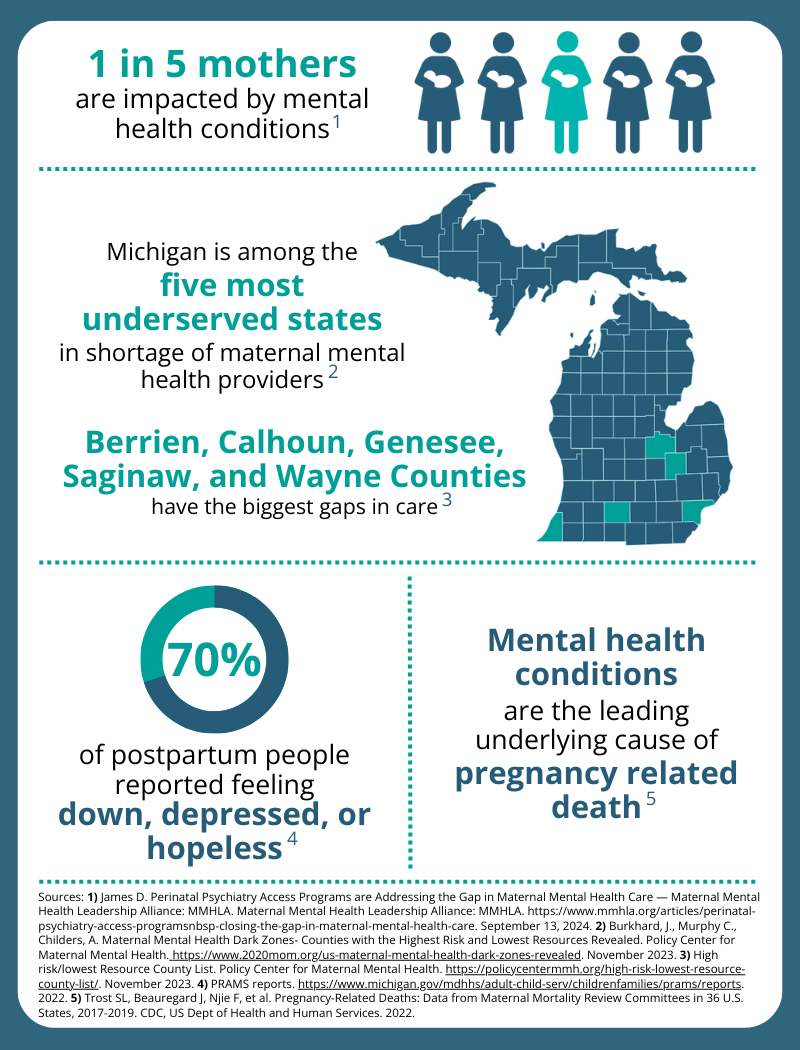
As we look ahead, we ask for your help in expanding this program’s reach. Please share this report with your colleagues so we can enroll more Michigan providers. Your insights are invaluable — what ideas do you have for how MC3 can better support providers and families?
Thank you for your dedication to this vital work. Together, we can build a future where no family faces the challenges of perinatal mental health alone, and every provider feels equipped and supported to deliver the care their patients need.
Michigan Clinical Consultation & Care (MC3) provides consultation, education, and linkages to community resources to build the capacity of Michigan’s primary care providers to respond to the behavioral health needs of pediatric and perinatal patients. MC3 is unique in that it is one of only a few Psychiatry Access Programs (PAPs) that houses both pediatric and perinatal together in one program.


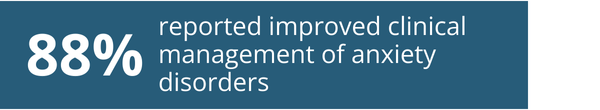
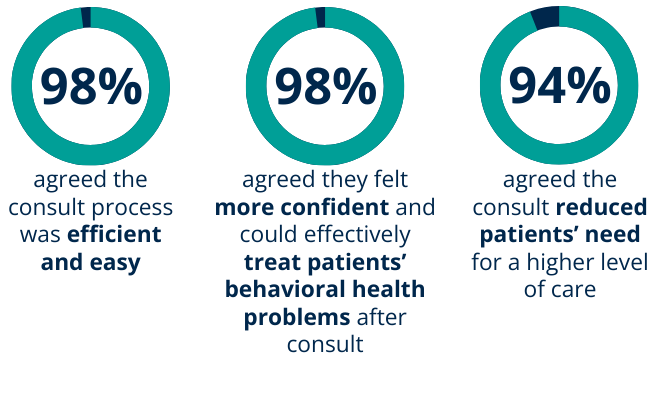
As a result of MC3 consultations, providers report increased confidence in diagnosing the most common behavioral conditions:
As a result of attending MC3 training “Youth Suicide Prevention in the Primary Care Setting,” providers report increased confidence in treating adolescents through:

MC3 perinatal patients experienced a 38% reduction in clinical depression and anxiety in their first month of services
Perinatal Patient Care service only available in select counties
Child & Adolescent Psychiatrists (CAPs) are integral to the improvement of our mental health crisis as they specialize in the diagnosis and treatment of behavioral and mental health disorders affecting youth. However, there is a severe shortage of CAPs both nationally and in the state of Michigan.
MC3 works to expand the reach of this specialized psychiatry by educating health care providers in Michigan on how to identify, treat, and manage behavioral and mental health concerns among youth. This is accomplished through MC3’s direct psychiatry consultations to discuss complex patients, educational trainings on behavioral/mental health topics, and digital library of free resources tailored to health care providers, including Psychopharmacology Reference Cards and Pediatric Resource Library.
The importance of mental health among perinatal people cannot be overstated. In addition to affecting the life of the pregnant person, research has demonstrated the presence of perinatal mental health disorders have been shown to increase the risk for psychological and developmental concerns in their children as well.
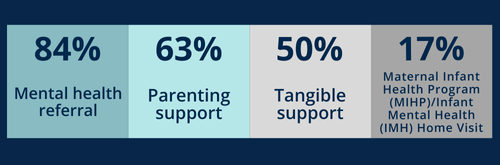
As a Perinatal Psychiatry Access Program (PPAP), MC3 ensures providers are equipped to support the needs of perinatal patients by educating front-line providers on the diagnosis and treatment of perinatal mental health conditions, consulting with providers on complex cases, and referring providers to local resources for support. Additionally, MC3 directly supports perinatal people through our infant mental health informed Perinatal Patient Care services, offered in select counties.


Data gathered from 2016-2024
MC3 and the Michigan Medicine Department of Psychiatry thank the Michigan Department of Health and Human Services (MDHHS), Medicaid Administration, and Health Resources and Services Administration for funding this work.