Kara Kucinski |
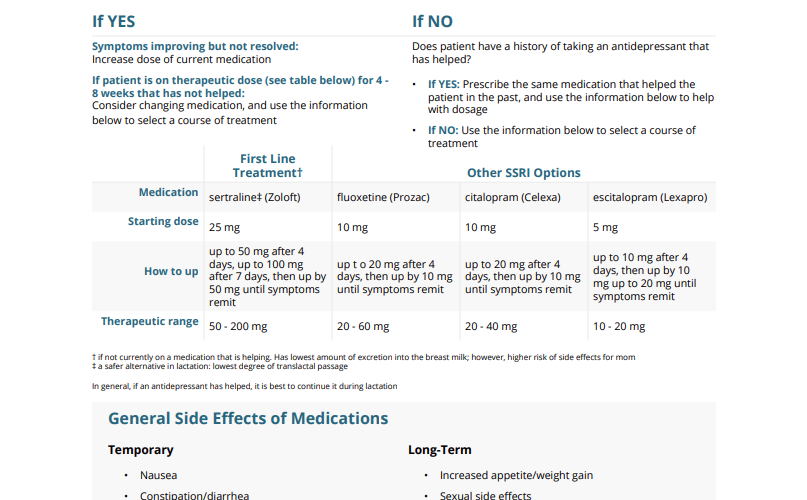
Symptoms improving but not resolved: Increase dose of current medication
If patient is on therapeutic dose (see table below) for 4 – 8 weeks that has not helped: Consider changing medication, and use the information below to select a course of treatment
Does patient have a history of taking an antidepressant that has helped?
• If YES: Prescribe the same medication that helped the patient in the past, and use the information below to help with dosage
• If NO: Use the information below to select a course of treatment
First Line Treatment
Other SSRI Options
Medication
sertraline (Zoloft)
fluoxetine (Prozac)
citalopram (Celexa)
escitalopram (Lexapro)
Starting dose
25 mg
10 mg
10 mg
5 mg
How to up
up to 50 mg after 4 days, up to 100 mg after 7 days, then up by 50 mg until symptoms remit
up to 20 mg after 4 days, then up by 10 mg until symptoms remit
up to 20 mg after 4 days, then up by 10 mg until symptoms remit
up to 10 mg after 4 days, then up by 10 mg up to 20 mg until symptoms remit
Therapeutic range
50 – 200 mg
20 – 60 mg
20 – 40 mg
10 – 20 mg
In general, if an antidepressant has helped, it is best to continue it during lactation
Temporary
Long-Term
Recommend patients take medication with food to decrease side effects Tell women only to increase dose if tolerating; otherwise wait until side effects dissipate before increasing For effects on fetus/neonate, see Discussing Antidepressant Use with Perinatal Patients.
2. Repeat EPDS in 2 – 4 weeks and re-evaluate depression treatment plan via clinical assessment
If no/minimal clinical improvement after 4-8 weeks
If clinical improvement and no/minimal side effects
If patient has no or minimal side effects, increase dose If patient has side effects that are severe/intolerable, or that do not resolve after 1-2 weeks, switch to a different medication
Reevaluate every month and at postpartum visit
This resource has been adapted with permission from the MCPAP for Moms Pediatric Toolkit for Postpartum Depression.
No Comments |
Kara Kucinski |
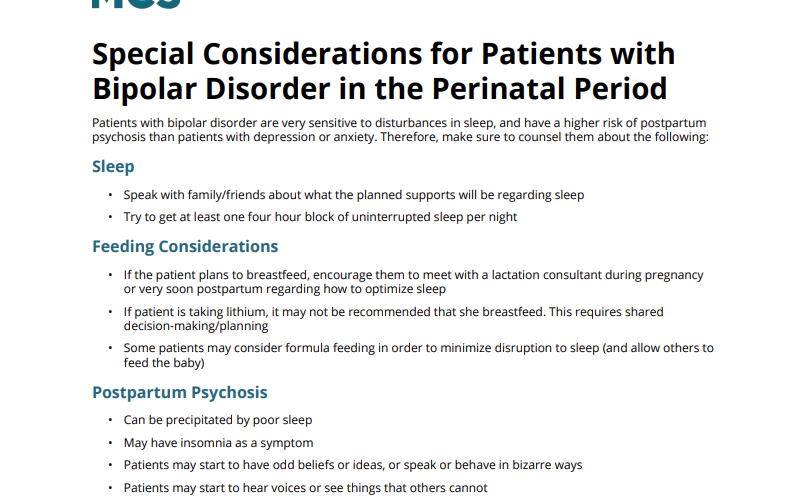
Patients with bipolar disorder are very sensitive to disturbances in sleep, and have a higher risk of postpartum psychosis than patients with depression or anxiety. Therefore, make sure to counsel them about the following:
No Comments |
Kara Kucinski |
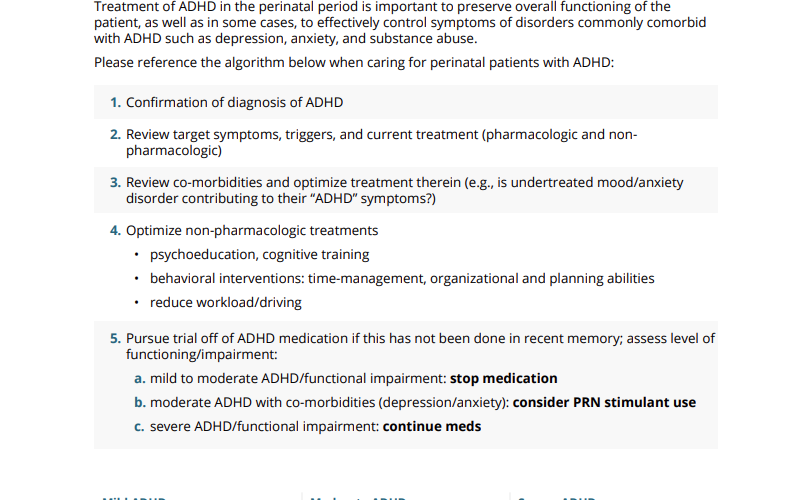
Treatment of ADHD in the perinatal period is important to preserve overall functioning of the patient, as well as in some cases, to effectively control symptoms of disorders commonly comorbid with ADHD such as depression, anxiety, and substance abuse.
Please reference the algorithm below when caring for perinatal patients with ADHD:
Mild ADHD (Minimal Functional Impairment Off Medication)
Moderate ADHD (Some Functional Impairment Off Medication)
Severe ADHD (Significant Functional Impairment, Including Driving)
Optimize sufficient non-pharmacologic management strategies and ensure self-management strategies in place
Optimize non-pharmacologic strategies; consider when necessary use of stimulant
Maintain medication, consider closer obstetric monitoring for fetal growth and hypertensive disorders of pregnancy
No Comments |
Kara Kucinski |
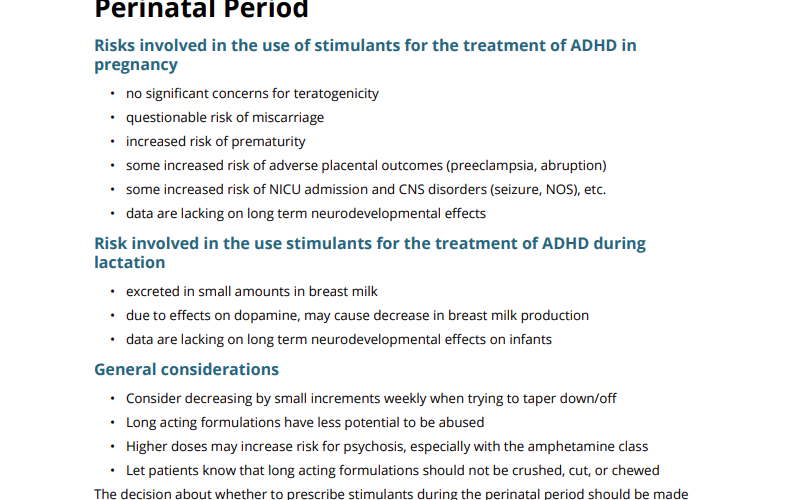
The decision about whether to prescribe stimulants during the perinatal period should be made jointly with the patient after sharing information about the risks and benefits. For a good review article and demonstration of shared decision-making, please reference this article:
No Comments |
Kara Kucinski |
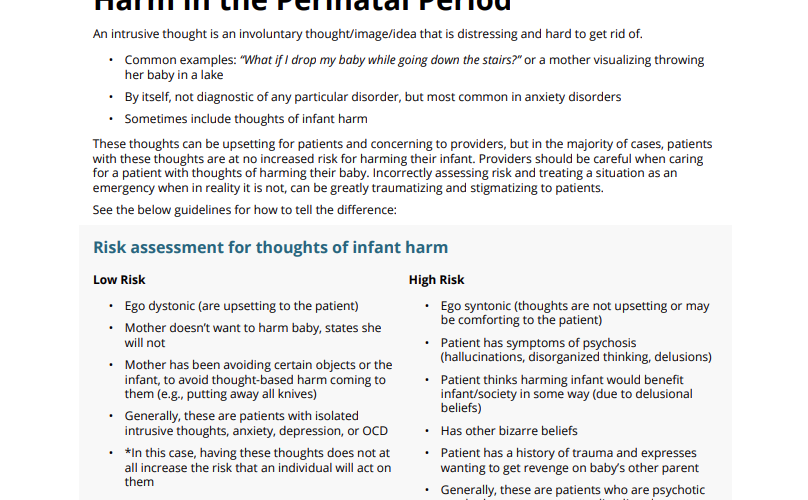
An intrusive thought is an involuntary thought/image/idea that is distressing and hard to get rid of.
These thoughts can be upsetting for patients and concerning to providers, but in the majority of cases, patients with these thoughts are at no increased risk for harming their infant. Providers should be careful when caring for a patient with thoughts of harming their baby. Incorrectly assessing risk and treating a situation as an emergency when in reality it is not, can be greatly traumatizing and stigmatizing to patients.
See the below guidelines for how to tell the difference:
Low Risk
High Risk
For more information, please watch MC3’s Intrusive Thoughts and OCD in the Perinatal Period recorded educational presentation.
No Comments |
Kara Kucinski |
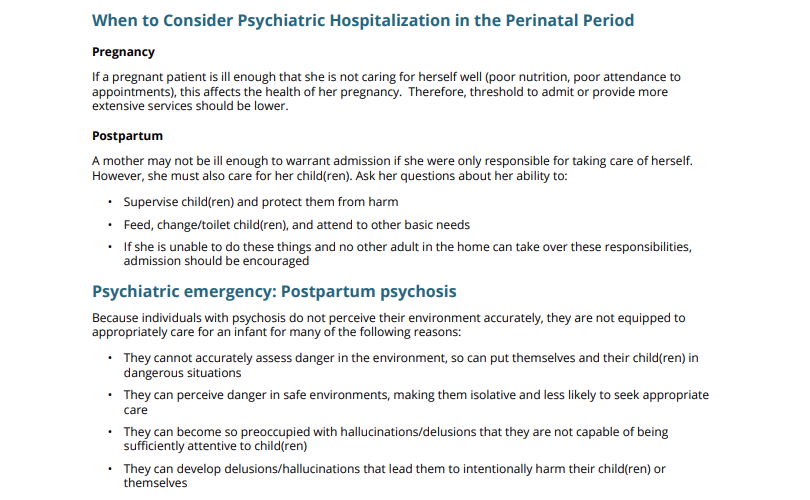
Pregnancy
If a pregnant patient is ill enough that she is not caring for herself well (poor nutrition, poor attendance to appointments), this affects the health of her pregnancy. Therefore, threshold to admit or provide more extensive services should be lower.
Postpartum
A mother may not be ill enough to warrant admission if she were only responsible for taking care of herself. However, she must also care for her child(ren). Ask her questions about her ability to:
Because individuals with psychosis do not perceive their environment accurately, they are not equipped to appropriately care for an infant for many of the following reasons:
For this reason, postpartum psychosis is a psychiatric emergency and requires admission.
No Comments |
Kara Kucinski |
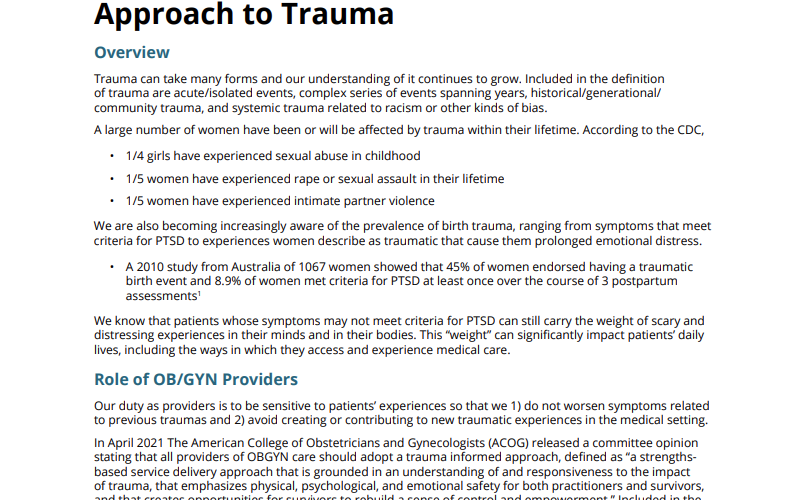
Trauma can take many forms and our understanding of it continues to grow. Included in the definition of trauma are acute/isolated events, complex series of events spanning years, historical/generational/ community trauma, and systemic trauma related to racism or other kinds of bias.
A large number of women have been or will be affected by trauma within their lifetime. According to the CDC,
We are also becoming increasingly aware of the prevalence of birth trauma, ranging from symptoms that meet criteria for PTSD to experiences women describe as traumatic that cause them prolonged emotional distress.
We know that patients whose symptoms may not meet criteria for PTSD can still carry the weight of scary and distressing experiences in their minds and in their bodies. This “weight” can significantly impact patients’ daily lives, including the ways in which they access and experience medical care.
Our duty as providers is to be sensitive to patients’ experiences so that we 1) do not worsen symptoms related to previous traumas and 2) avoid creating or contributing to new traumatic experiences in the medical setting.
In April 2021, The American College of Obstetricians and Gynecologists (ACOG) released a committee opinion stating that all providers of OBGYN care should adopt a trauma informed approach, defined as “a strengths-based service delivery approach that is grounded in an understanding of and responsiveness to the impact of trauma, that emphasizes physical, psychological, and emotional safety for both practitioners and survivors, and that creates opportunities for survivors to rebuild a sense of control and empowerment.” Included in the practice of trauma informed care are the following:
No Comments |
Kara Kucinski |
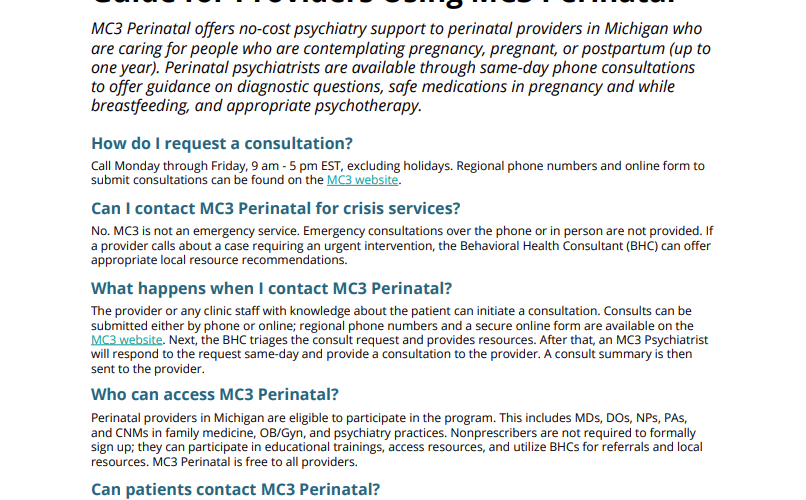
MC3 Perinatal offers no-cost psychiatry support to perinatal providers in Michigan who are caring for people who are contemplating pregnancy, pregnant, or postpartum (up to one year). Perinatal psychiatrists are available through same-day phone consultations to offer guidance on diagnostic questions, safe medications in pregnancy and while breastfeeding, and appropriate psychotherapy.
Call Monday through Friday, 9 am – 5 pm EST, excluding holidays. Regional phone numbers and online form to submit consultations can be found on the MC3 website.
No. MC3 is not an emergency service. Emergency consultations over the phone or in person are not provided. If a provider calls about a case requiring an urgent intervention, the Behavioral Health Consultant (BHC) can offer appropriate local resource recommendations.
The provider or any clinic staff with knowledge about the patient can initiate a consultation. Consults can be submitted either by phone or online; regional phone numbers and a secure online form are available on the MC3 website. Next, the BHC triages the consult request and provides resources. After that, an MC3 Psychiatrist will respond to the request same-day and provide a consultation to the provider. A consult summary is then sent to the provider.
Perinatal providers in Michigan are eligible to participate in the program. This includes MDs, DOs, NPs, PAs, and CNMs in family medicine, OB/Gyn, and psychiatry practices. Nonprescribers are not required to formally sign up; they can participate in educational trainings, access resources, and utilize BHCs for referrals and local resources. MC3 Perinatal is free to all providers.
No. The MC3 Perinatal phone line is only for providers; patients should not call MC3 Perinatal.
Providers also have access to the following: live and remote trainings offered regionally and statewide; workflow analysis to better integrate screening, care coordination, and MC3 services; local and regional behavioral health resource and referral navigation; and scheduled educational group case consultation with an MC3 Psychiatrist.
Visit the MC3 website to sign up.
No Comments |
Kara Kucinski |
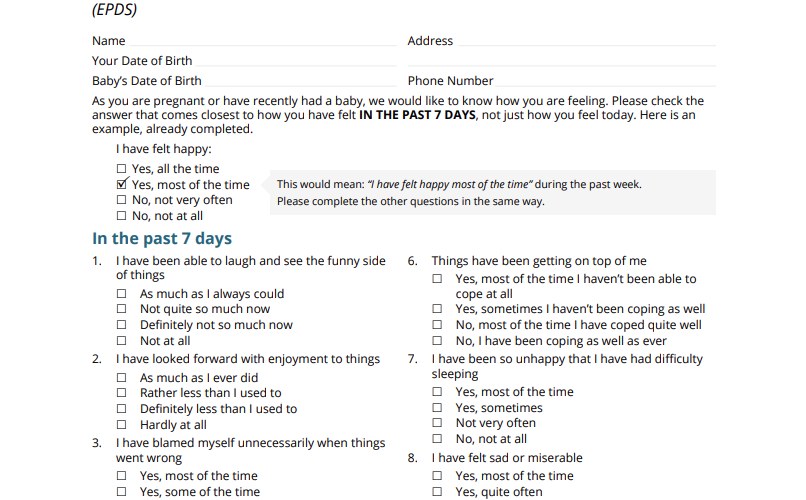
Name ______________________________________________
Your date of birth __________________________________
Baby’s date of birth ________________________________
Address ______________________________________________
Phone number _______________________________________
As you are pregnant or have recently had a baby, we would like to know how you are feeling. Please check the answer that comes closest to how you have felt IN THE PAST 7 DAYS, not just how you feel today. Here is an example, already completed.
I have felt happy:
Yes, all the time
Yes, most of the time
This would mean: “I have felt happy most of the time” during the past week.
No, not very often
No, not at all
6. Things have been getting on top of me
As much as I always could
Yes, most of the time I haven’t been able to cope at all
Not quite so much now
Yes, sometimes I haven’t been coping as well
Definitely not so much now
No, most of the time I have coped quite well
Not at all
No, I have been coping as well as ever
2. I have looked forward with enjoyment to things
7. I have been so unhappy that I have had difficulty sleeping
As much as I ever did
Yes, most of the time
Rather less than I used to
Yes, sometimes
Definitely less than I used to
Not very often
Hardly at all
No, not at all
3. I have blamed myself unnecessarily when things went wrong
8. I have felt sad or miserable
Yes, most of the time
Yes, most of the time
Yes, some of the time
Yes, sometimes
Not very often
Not very often
No, never
No, not at all
4. I have been anxious or worried for no good reason
9. I have been so unhappy that I have been crying
No, not at all
Yes, most of the time
Hardly ever
Yes, quite often
Yes, sometimes
Only occasionally
Yes, very often
No, never
5. I have felt scared or panicky for no very good reason
10. The thought of harming myself has occurred to me
Yes, quite a lot
Yes, quite often
Yes, sometimes
Sometimes
No, not much
Hardly ever
No, not at all
Never
Administered/Reviewed by _________________________________________
Date ___________________________________________
No Comments |
Kara Kucinski |
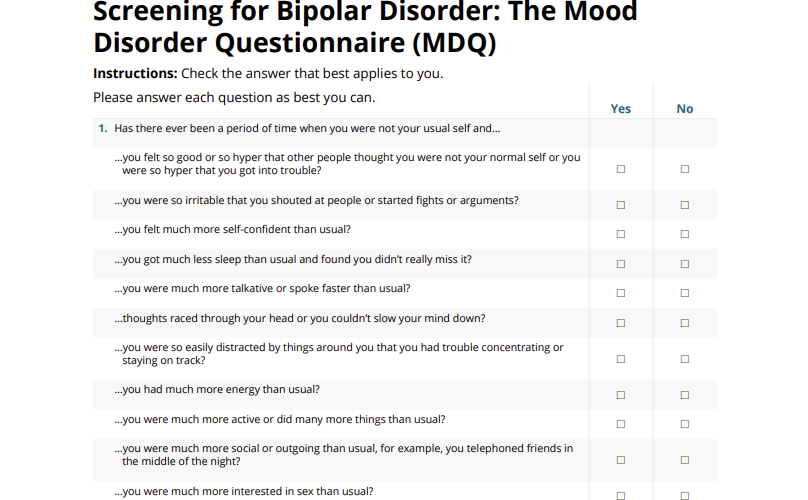
Instructions: Check the answer that best applies to you.
Please answer each question as best you can.
Yes
No
1.
Has there ever been a period of time when you were not your usual self and…
…you felt so good or so hyper that other people thought you were not your normal self or you were so hyper that you got into trouble?
…you were so irritable that you shouted at people or started fights or arguments?
…you felt much more self-confident than usual?
…you got much less sleep than usual and found you didn’t really miss it?
…you were much more talkative or spoke faster than usual?
…thoughts raced through your head or you couldn’t slow your mind down?
…you were so easily distracted by things around you that you had trouble concentrating or staying on track?
…you had much more energy than usual?
…you were much more active or did many more things than usual?
…you were much more social or outgoing than usual, for example, you telephoned friends in the middle of the night?
…you were much more interested in sex than usual?
…you did things that were unusual for you or that other people might have thought were excessive, foolish, or risky?
…spending money got you or your family in trouble?
2.
If you checked YES to more than one of the above, have several of these ever happened during the same period of time?
3.
How much of a problem did any of these cause you — like being able to work; having family, money, or legal troubles; getting into arguments or fights? Please check 1 response only.
No problem
Minor problem
Moderate problem
Serious problem
4.
Have any of your blood relatives (e.g., children, siblings, parents, grandparents, aunts, uncles) had manic-depressive illness or bipolar disorder?
5.
Has a health professional ever told you that you have manic-depressive illness or bipolar disorder?
This questionnaire should be used as a starting point. It is not a substitute for a full medical evaluation. Bipolar disorder is a complex illness, and an accurate, thorough diagnosis can only be made through a personal evaluation by your doctor.
This instrument is designed for screening purposes only and is not to be used as a diagnostic tool.
The questionnaire takes less than 5 minutes to complete. Patients simply check the yes or no boxes in response to the questions. The last question pertains to the patient’s level of functional impairment. The physician, nurse, or medical staff assistant then scores the completed questionnaire.
Further medical assessment for bipolar disorder is clearly warranted if patient:
No Comments |